A practice that recognises the profound influence of social, economic, and environmental factors on health, social prescribing offers a holistic approach to wellbeing. By connecting individuals with community resources - from cooking lessons to fitness clubs - it empowers people to take control of their health beyond the doctor's office.
This article explores the roots, mechanisms, benefits, and the broad acceptance of social prescribing within the UK, shedding light on how this approach is reshaping the landscape of healthcare by looking at the bigger picture while turning inwards to tap into the power of the community.
What is social prescribing?
When we’re unwell, we go to the GP. This is in spite of the fact that many chronic conditions whic might lead us to the doctor's surgery are linked to our surroundings, diet, and lifestyle. These, in turn, can be traced back to social, economic, and environmental factors.
Social prescribing takes a step back from the linear route to the GP surgery when we’re sick, and takes a more holistic approach to health and wellbeing.
It draws on existing resources in the community, such as financial advice, cooking lessons, and fitness clubs, and connects people to these services or groups to allow them to manage and take charge of their health. Social prescribing can even support people in starting their own services or groups in the absence of a relevant option.
Also known as community referral, social prescribing, while linking in with the NHS, is a non-clinical service, and mostly focuses on mental, emotional, and physical wellbeing. Given that non-communicable diseases (NCDs), often known as “lifestyle” diseases, are responsible for around 89% of deaths in the UK, the power of this alternate route to improved health is not to be underestimated.
Since the term is quite broad in scope, as it could describe a structured path of care or a more flexible approach in signposting, some core principles were needed to guide the practice as it has gained more attention in recent years.
These are that social prescribing:
is a holistic approach focussing on individual need
promotes health and wellbeing and reduces health inequalities in a community setting, using non-clinical methods
addresses barriers to engagement and enables people to play an active part in their care
utilises and builds on the local community assets in developing and delivering the service or activity
aims to increase people’s control over their health and lives
To paraphrase the a panel of experts' description of social prescribing, the practice is a way for “trusted individuals in clinical and community settings” to identify when someone has a social need that affects their health, and connect them to services within the community.
“a means for trusted individuals in clinical and community settings to identify that a person has non-medical, health-related social needs,
and to subsequently connect them to non-clinical support and services within the community by co-producing a social prescription: a non-medical prescription to improve health and wellbeing, and to strengthen community connections.”
- Global Social Prescribing Alliance: International Playbook
How is social prescribing put into practice?
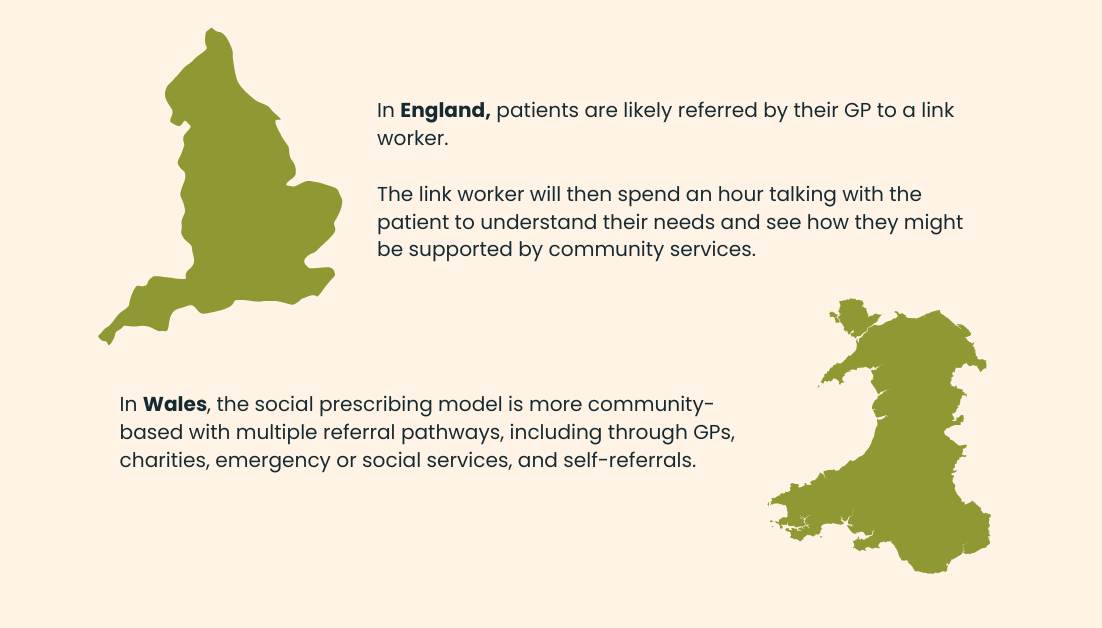
The process looks a little different depending on where you are. In England, patients are likely referred by their GP to a link worker. The link worker will then spend an hour talking with the patient to understand their needs and see how they might be supported by community services.
GPs themselves often have experience in social prescribing (80% of them, according to Government figures). However, the 10-minute appointment window is not enough time to discuss issues in depth, which is where the link worker comes in.
In Wales, the social prescribing model is more community-based as opposed to England’s typical route through the healthcare system. The “All Wales Model of Social Prescribing” has multiple referral pathways, including through GPs, charities, emergency or social services, and self-referrals.
In the case of supported referrals, the professional who puts the person in touch with relevant services and offers continued encouragement has many names. Social prescriber, link worker, support broker, or community navigator are just a few of the reported 75 terms used in the UK.
Based on initial discussions, the link worker might introduce the patient to a new activity or club, guidance, or a charity that could provide volunteers who can support the individual in another way, such as doing their shopping. They would tap into their knowledge or local resources that would be a good fit.
Instead of simply being prescribed medication to relieve anxiety or low mood, or being given a leaflet about healthy eating at a doctor's appointment, the individual could be directed to a way in which they can address the root cause of their symptoms, and be supported throughout this introduction.
For instance, someone might be worried about their finances and lack the skills and confidence to cook healthy meals on a budget at home. A social prescriber could direct them to a charity that offers free financial advice, and a group that gives healthy cooking lessons once a week.
What are the benefits of social prescribing?
Studies have linked social prescribing to improved emotional, physical, and mental well-being through qualitative data based on patients’ experiences. An evaluation report from the University of Westminster drew on perceptions from patients in Shropshire who had been referred to social prescribing, and welcomed positive comments about the level of attention offered through this approach:
I think partly the attraction of it was that there was somebody who was happy to talk about my problem and also say, I can give you an hour.
If they hadn’t persisted I’d have just forgotten about it. If it had just been one visit to the surgery I’m sure…there would have been a very different outcome
Other studies from the University of Westminster suggest a 28% reduction in the number of GP appointments for individuals supported by social prescribing, and a 24% drop in A&E visits.
Meanwhile, the British Journal of Medical Practice warned in their report Social Prescribing: Where is the evidence? that it’s hard to measure the success of social prescribing because every program is different and depends a lot on where it's happening.
The authors of the report suggest that to really understand how well social prescribing works, it needs to be studied as a whole system that includes many parts, like the activities offered and the workers who link patients to these activities. Instead of focussing on how social prescribing improves health directly, studies could examine how it affects people's experiences and fits into their lives.
But even in that same report, it was clear that a more holistic approach to wellbeing was necessary, as it's believed that about 1 in 5 people go to their doctor mostly for problems that are more about their life and social situations than medical issues.
Because we have more older people, more people with complicated health and social needs, and more pressure on health services, the idea of social prescribing, where doctors suggest non-medical help, is becoming more popular.
A study published in 2023 by The Department of Health and Social Care (DHSC) showed that clinicians widely believe that green social prescribing can notably improve mental health (87%), along with enhancing physical health, empowering patient self-care, reducing health inequalities, and alleviating healthcare system pressures.
And organisations such as The National Academy for Social Prescribing (NASP), are helping to support the growing body of evidence to state an economic case for social prescribing.
They have shared 13 studies indicating that social prescribing can help save money and lessen the workload on the healthcare system. To highlight the financial advantages of social prescribing, a quick review was done of 26 studies about its economic and healthcare usage impacts. The findings reveal that social prescribing can be cost-effective, with returns ranging from £2.14 to £8.56 for every £1 spent.

How long has it been around?
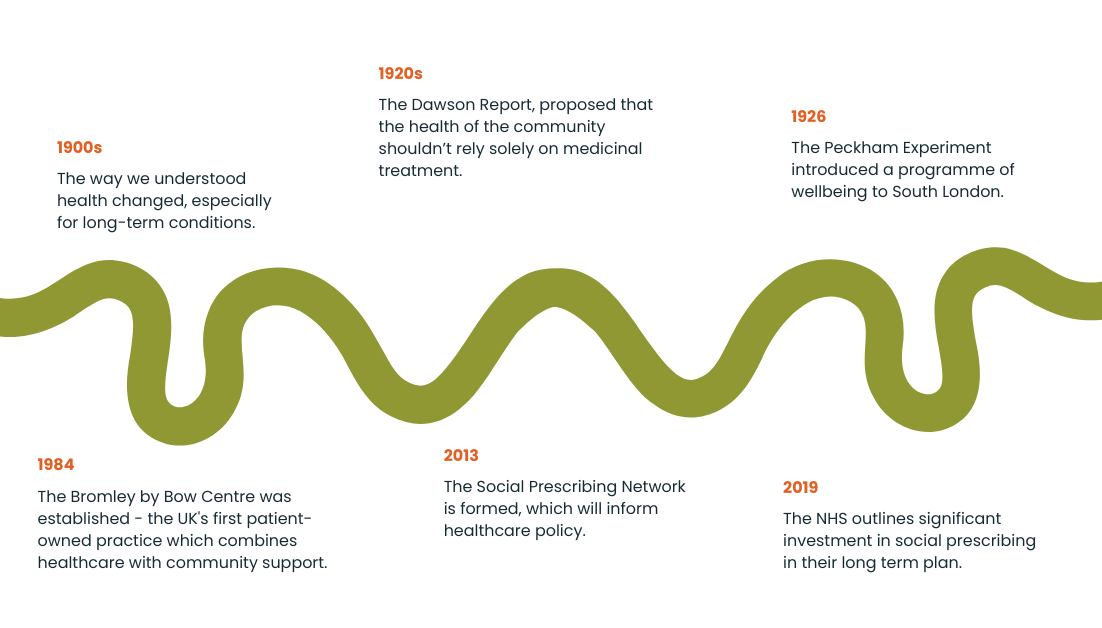
Since the 1990s, the way we understand health, especially for long-lasting illnesses like back and neck pain, has changed. We now consider not just the physical aspects but also the psychological and social factors. This shift led to new types of health programs, such as social prescribing, which includes activities like art classes, exercise programs, walking groups, and health coaching. These programs are designed to help people manage their illnesses, prevent more serious problems, and build community support, particularly as the population gets older and more people live with chronic conditions.
The Social Prescribing Network’s co-founder Dr. Michael Dixon suggests that we could go as far back as the 1920’s Dawson Report, which proposed that the health of the community shouldn’t rely solely on medicinal treatment. Six years after the report’s release, the Peckham Experiment encouraged families in south London to take charge of their wellbeing from 1926-1950 with a programme of exercise.
Fast forward three decades, and the Bromley by Bow Centre emerged in the mid-1980s in Tower Hamlets when a local priest joined community volunteers to address severe inequalities. The charity expanded to offer various community services and established a unique GP practice by 1997. This practice, which focussed on addressing the social factors affecting health, was the UK's first patient-owned practice and today combines healthcare with community support to empower patients and improve health outcomes by integrating services.
Social prescribing as we have come to know it today began to take shape when research conducted since 2013 by Dr Michael Dixon, Dr. Marie Polley, Dr. Alison Fixsen, Professor Damien Ridge, and Dr. Karen Pilkington, culminated in the creation of the Social Prescribing Network, which has influenced healthcare policy since.
Six years later, in 2019, the NHS outlined its commitment to increasing access to social prescribing for everyone in the UK, in the NHS Long Term Plan, signalling “the biggest investment in social prescribing by any national health system”.
This is the biggest investment in social prescribing by any national health system and legitimises non-medical community-based activities and holistic support alongside medical treatment as part of a personalised care approach.
- NHS
How Ayup Connect supports social prescribing
Right around the time that the NHS announced its plans for an increased focus on social prescribing, Kingston Council had been conducting its own research on how to upstream support and concluded that they needed a way to allow residents to self-refer to support services.
At Ayup Digital, we worked with Kingston Council on what would become the first deployment of our Ayup Connect platform, a directory of community support services that made it easy for residents to find and connect with organisations that could offer them help.
2023 figures showed that just over 22% of the borough’s population were taking advantage of this community asset, with over 37,810 visitors to the council platform, Connected Kingston.
These visits resulted in 16,570 searches, 95% of which returned one or multiple services.
The most frequently searched terms in 2023 tied into social connections, which drew in searches around words like “friend”, “social” and “lonely”. After that, the most popular searches were linked to Mental Health. This was followed by terms relating to health and fitness, including searches such as “weight loss” as well as those relating to specific activities including “walking”, “yoga” and “swim”.
The self-referral approach facilitated by Ayup Connect empowers residents to take control over their health and wellbeing while helping build a stronger community by connecting people to the groups that can help them live their best lives.
But, the platform is for link workers too, providing them with up-to-date information on services, all in one place, so they are better equipped to support patients who have been referred to them by their GP.
Conclusion
There’s little doubt as to why the NHS is planning to invest so heavily in social prescribing, while the Welsh public health service is launching a dedicated national framework. Social prescribing represents a transformative approach to healthcare that shifts focus from purely medical treatments to a holistic model addressing the physical, psychological, and social determinants of health.
Connecting individuals with community resources and activities not only empowers them to take charge of their health and wellbeing but also demonstrates significant potential in reducing healthcare costs and alleviating pressures on the healthcare system.
This new approach, which has a deep-rooted understanding of how health and social issues are linked, has evolved over the decades. It is now getting the support and attention it needs, showing a promising path towards a responsive and more connected way of looking after people's health.
To find out how Ayup Connect can support your residents with relevant information and the option to self-refer, get in touch with our team at Ayup Digital.
